How 3D Printing With Flexible Filaments Creates Revolutionary Custom Orthotics

Dr. Emma Reynolds, DPM
Biomechanics Researcher & Orthotic Specialist
The field of orthotic design has historically faced a fundamental challenge: how to create devices that provide rigid support in some areas while remaining flexible and accommodating in others. Traditional manufacturing methods require using multiple materials laminated together or complex fabrication processes to achieve variable firmness within a single orthotic device. Now, 3D printing custom foot orthotics with advanced flexible filaments is revolutionizing this approach, enabling the creation of truly customized devices with precisely controlled density zones—all from a single material in a single printing process.
The Limitations of Traditional Orthotic Design
To understand the revolutionary nature of this development, it's important to recognize the constraints that have shaped orthotic design for decades:
The Density Dilemma
Traditional orthotics typically fall into one of two categories: rigid functional devices that provide stability and control motion, or soft accommodative devices that offer cushioning and pressure redistribution. Attempts to create orthotics that combine both properties have typically relied on:
- Material Layering: Bonding materials of different densities (such as a rigid polypropylene shell with softer EVA or poron top covers)
- Selective Grinding: Thinning specific areas of a material to create zones of greater flexibility
- Posting Techniques: Adding firmer materials to specific areas to create support structures
These approaches involve multiple materials, multiple manufacturing steps, and often result in visible seam lines or abrupt transitions between density zones—all of which can affect both comfort and durability.
The Customization Challenge
Even with advanced traditional fabrication techniques, creating truly personalized density patterns based on individual patient biomechanics has been prohibitively complex. The manual processes involved make it impractical to create fine-tuned density variations that precisely match a patient's unique pressure distribution patterns.
The 3D Printing Revolution: Variable Density from a Single Material
3D printing custom foot orthotics with flexible filaments—particularly Thermoplastic Polyurethane (TPU) and its specialized medical-grade variants—has introduced a paradigm shift in how we approach orthotic design. The key innovation lies in the printer's ability to control the internal structure of the device at a microscopic level, creating varying degrees of flexibility or rigidity using the same material throughout.
Understanding Infill Density and Pattern Control
When creating flexible filament orthotics, the 3D printer doesn't simply produce a solid object. Instead, it builds the orthotic with carefully designed internal structures that determine how the device responds to pressure. This is achieved through two primary controls:
- Infill Density: The percentage of the internal volume filled with material. Higher percentages (such as 80-100%) create firmer, more supportive regions, while lower percentages (20-50%) create more flexible, cushioned areas.
- Infill Pattern: The geometric arrangement of the internal material. Patterns like triangular or honeycomb provide structural support, while patterns like gyroid or cubic offer more flexible cushioning with excellent energy return properties.
These parameters can be precisely controlled within different regions of the same orthotic, all while maintaining a seamless exterior surface. The result is a device that can be rigid exactly where stability is needed and flexible precisely where cushioning is required—all created in a single printing process using a single material.

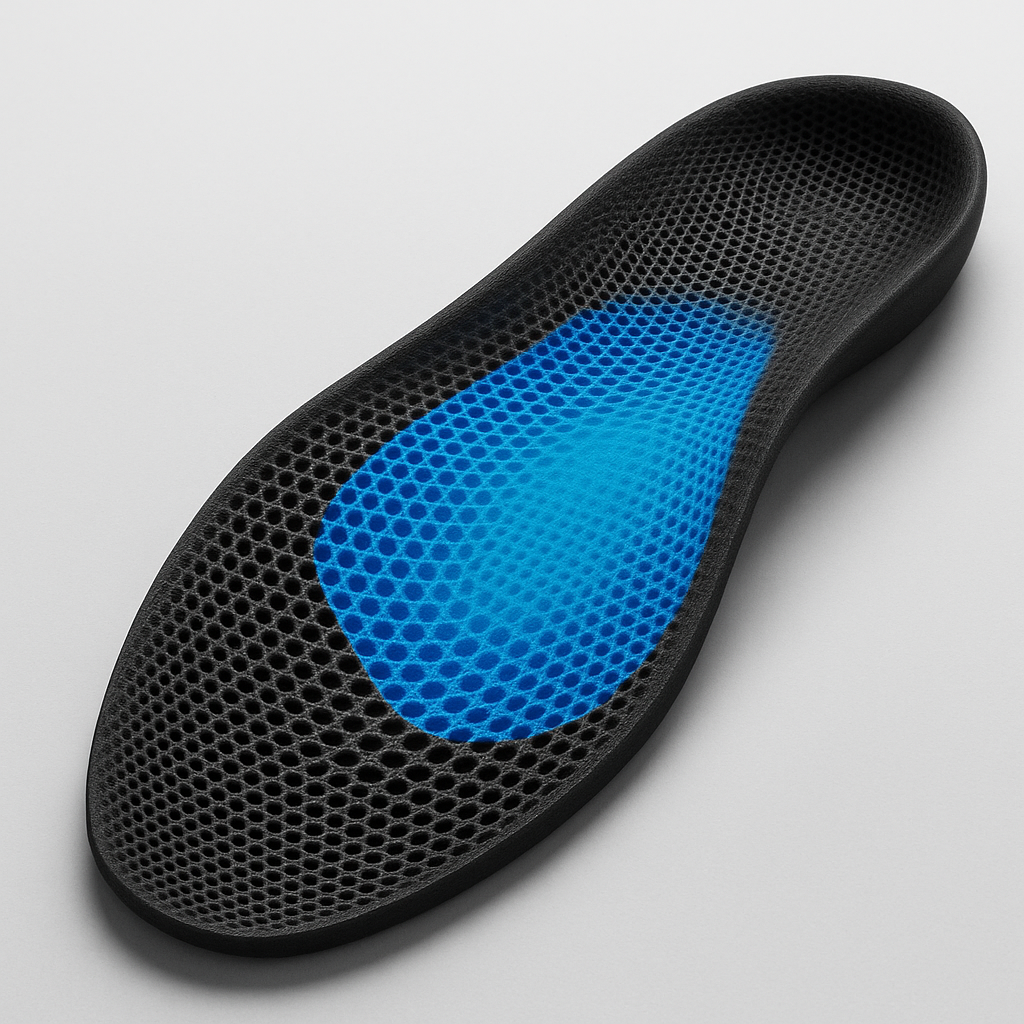
Traditional orthotic using multiple bonded materials to achieve variable support

3D printed orthotic with seamless variable density controlled by internal structure
Clinical Benefits of Variable Density 3D Printed Orthotics
The ability to create variable density orthotics within a single device and material opens up new clinical possibilities that were previously difficult or impossible to achieve:
Truly Biomechanically Optimized Support
Rather than simply choosing between rigid or soft orthotics, clinicians can now prescribe devices with precisely tailored support characteristics:
- Firm arch support that transitions gradually to a more flexible forefoot for improved propulsion during gait
- Rigid heel cup and midfoot for stability combined with softer zones under pressure-sensitive areas like metatarsal heads
- Targeted pressure relief for specific conditions such as neuromas or plantar lesions without compromising overall support
- Gradient firmness patterns that follow the unique pressure distribution map of the individual patient
Dr. Mark Stevens, a podiatrist who has been prescribing custom TPU orthotics for three years, notes: "The ability to create smooth transitions between support zones has been game-changing for my patients with complex biomechanical issues. We're seeing better clinical outcomes because we're no longer forced to compromise between support and comfort—we can optimize for both simultaneously."
Improved Comfort and Compliance
Patient comfort and the resulting compliance with orthotic therapy is significantly enhanced with variable density orthotics:
- Elimination of harsh transitions between materials that can cause irritation or "edge effect" discomfort
- Enhanced shock absorption in specific areas without compromising control elsewhere
- Better adaptation to changing foot dynamics during different phases of gait
- Reduced break-in period as the orthotic can provide rigid support while still accommodating to the foot's contours
These comfort advantages translate directly to higher compliance rates, as patients are more likely to wear devices that don't cause discomfort or require extensive adaptation periods.
Durability Advantages
3D printed orthotics with variable density zones offer unique durability benefits compared to traditional multi-material devices:
- No delamination: Since the entire orthotic is a single continuous piece of material, there are no layers that can separate over time
- Consistent performance: The material properties remain stable throughout the life of the device
- Predictable wear patterns: The orthotic tends to wear more uniformly without the differential breakdown often seen at the junction of different materials
- Water and chemical resistance: Many TPU filaments offer excellent resistance to moisture and common environmental contaminants
These durability factors contribute to longer-lasting devices that maintain their therapeutic effectiveness throughout their lifespan.
The Technical Evolution: How We Got Here
The ability to create multi-density orthotic devices using a single material has emerged from several converging technological advances:
Advanced Orthotic-Specific Filaments
The development of medical-grade flexible filaments has been crucial to making variable density 3D printing viable for orthotic applications:
- Specialized TPU formulations designed specifically for orthotic applications, with carefully calibrated hardness ratings (typically 85-95A Shore hardness)
- Biocompatible materials that meet medical device standards for skin contact
- Enhanced elasticity that provides both compression resistance and energy return
- Improved thermal stability during printing, allowing for more precise control of internal structures
These materials provide the foundation upon which variable density printing techniques can be successfully applied to orthotic production.
Advanced Slicer Software
Equally important has been the development of sophisticated "slicer" software that prepares 3D models for printing:
- Zone-specific parameter control allowing different infill densities and patterns within a single model
- Gradient transitions that create smooth density changes between zones
- Integration with pressure mapping data to automatically generate density patterns based on individual patient measurements
- Machine learning algorithms that optimize internal structures based on biomechanical principles and patient-specific factors
Modern orthotic design software can now automatically generate these complex variable density structures based on the clinician's prescription parameters and patient-specific scan data, making the technology accessible even to practitioners without extensive 3D printing expertise.
Clinical Applications and Case Studies
The clinical applications of variable density orthotics through flexible filament 3D printing are vast and continue to expand as practitioners gain experience with the technology:
Case Study 1: The Athlete with Midfoot Pain
A 28-year-old competitive runner presented with midtarsal joint pain exacerbated during the propulsive phase of gait. Traditional rigid orthotics provided adequate support but increased forefoot pain, while softer devices failed to control excessive midfoot motion.
Using flexible filament orthotics with 3D printing, a device was created with:
- 90% infill density with triangular pattern in the medial arch for rigid support
- Gradual transition to 50% infill with gyroid pattern in the forefoot for flexibility during toe-off
- 70% infill with specialized cushioning pattern under the specific painful joints
The runner reported immediate comfort, resumed training within one week, and returned to competition level performance within three weeks—all while wearing a single pair of orthotics for both training and competition.
Case Study 2: The Diabetic Patient with Multiple Pressure Points
A 62-year-old patient with diabetes presented with multiple plantar pressure points and a history of previous ulceration. The challenge was creating a device that offloaded pressure areas while providing sufficient support to control pronation that was contributing to the pressure issues.
A custom TPU orthotic was designed with:
- Firm (85% infill) midfoot and heel cup for stability
- Very soft (30% infill) precisely mapped zones corresponding exactly to elevated pressure areas identified through scanning
- Moderate support (60% infill) in transition zones providing a gradual change in density
Pressure mapping performed while wearing the orthotics showed pressure reduction of over 40% at critical sites, while maintaining overall foot stability. After six months, no new lesions had developed, and existing calluses had reduced significantly.
Implementing Variable Density Printing in Practice
For medical professionals interested in implementing variable density orthotics in their practice, several important considerations should guide technology selection and workflow development:
Equipment Requirements
Not all 3D printers are capable of producing high-quality variable density medical devices. Key requirements include:
- Direct drive extruder systems capable of precisely controlling flexible filament flow
- Temperature-controlled build chambers to ensure consistent material properties throughout the print
- High-resolution capability (minimum 0.1mm layer height) for smooth transitions between density zones
- Reliable, repeatable performance essential for medical device production
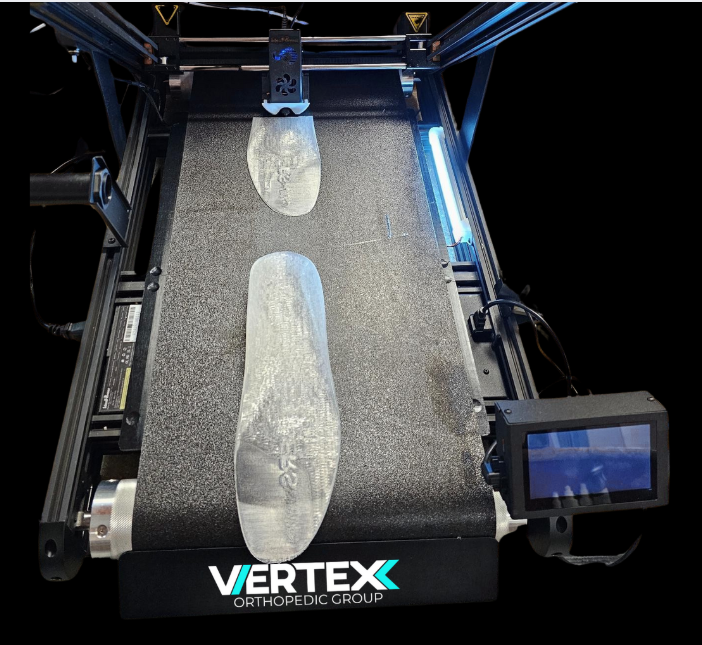
Purpose-built medical 3D printers like the Vertex Apex Belt V2 are specifically designed to meet these requirements for orthotic 3D printing applications.
Design Software and Workflow Integration
The design process for variable density orthotics typically follows this workflow:
- Patient assessment and 3D scanning to capture foot morphology
- Pressure mapping to identify areas requiring specific density modifications
- Base orthotic design creation in specialized orthotic CAD software
- Density zone mapping where the clinician defines regions requiring different properties
- Slicing with zone-specific parameters to create the final print instructions
- Production and minimal finishing to prepare the device for dispensing
Modern orthotic design software platforms increasingly incorporate automated density zone mapping based on pressure data, simplifying this process for clinicians.
The Future of Variable Density Orthotic Design
As flexible filament orthotics technology continues to evolve, several emerging trends point to even more sophisticated applications:
AI-Driven Biomechanical Optimization
Machine learning algorithms are beginning to analyze thousands of successful orthotic designs alongside patient outcomes to suggest optimal density patterns based on specific diagnostic criteria and patient characteristics. These systems continue to improve as they incorporate more data, creating increasingly effective density distribution models.
Dynamic Response Tuning
Beyond simple soft or firm zones, research is advancing in designing internal structures that provide specific response characteristics—such as energy return during specific phases of gait or progressive resistance that changes with applied force. These developments promise orthotics that actively assist movement rather than simply supporting static structure.
Multi-Material Variable Density Printing
While single-material variable density printing offers tremendous advantages, the next frontier involves multi-material 3D printers that can combine different flexible filaments within a single device—allowing even greater control over performance characteristics while maintaining seamless construction.
Patient-Directed Optimization
Perhaps most exciting is the potential for iterative optimization based on patient feedback. The digital nature of 3D printing allows clinicians to make precise adjustments to density patterns between versions, gradually refining the design to achieve optimal outcomes for complex cases.
Conclusion: A New Paradigm in Orthotic Therapy
3D printing custom foot orthotics with variable density through flexible filaments represents much more than an incremental improvement in fabrication techniques—it's a fundamental shift in how we conceptualize orthotic therapy. By eliminating the traditional dichotomy between rigid functional devices and soft accommodative ones, this technology opens new possibilities for truly personalized care that optimizes both biomechanical control and patient comfort.
As clinicians gain experience with this approach and the supporting technologies continue to advance, variable density 3D printed orthotics will likely become the new standard of care—offering better outcomes, improved patient satisfaction, and new treatment possibilities for even the most challenging cases.
For medical professionals who have struggled with the limitations of traditional orthotic design, the ability to create seamless, precisely controlled density transitions within a single device represents nothing less than a revolution in orthotic therapy—one that benefits both practitioners and patients through unprecedented customization capabilities.

About the Author
Dr. Emma Reynolds is a board-certified podiatrist specializing in biomechanics and sports medicine. She has published numerous research papers on advanced orthotic design and serves as a consultant for several medical technology companies developing next-generation orthotic solutions.
Related Articles
How In-Office 3D Printing Reduces Wait Times for Custom Insoles
Learn how 3D printing technology is revolutionizing patient care by enabling same-day custom orthotics.

CNC Milling vs. 3D Printing: Which Is Better for Custom Orthotics?
A comprehensive comparison of the two leading technologies for in-office orthotic production.
Stay Updated on Orthotic Technology
Subscribe to our newsletter for the latest insights on 3D printing custom foot orthotics, variable density design, and clinical best practices.